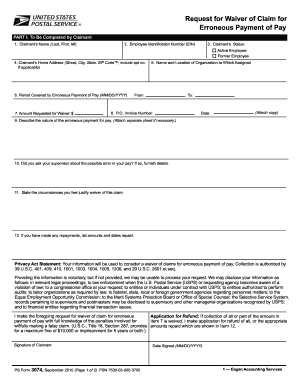
Texas Medicaid Hospice Program Form 3074 Hospice
Texas Administrative CodeTexas Administrative CodeADMINISTRATIONTEXAS HEALTH AND HUMAN SERVICES COMMISSIONMEDICAID AND OTHER HEALTH AND HUMAN SERVICES FRAUD AND ABUSE PROGRAM INTEGRITYUTILIZATION REVIEWRULE §371.214Resource Utilization Group Classification System(a) The Resource Utilization Group (RUG-III) 34-group classification system has seven major classification groups. The groups represent the recipient's relative direct care resource requirements. (b) The Activities of Daily Living (ADL) score is based on the recipient's care needs that are provided by the nursing facility staff. The ADL score is used to determine a recipient's placement in a RUG-III category and is based on the recipient's care needs provided by the nursing facility staff. The score is incorporated into acuity measurements established under the RUG-III recipient classification methodology. The clinical record must support items claimed for Medicaid reimbursement on the Minimum Data Set (MDS).
(c) The state-specific Long-Term Care Medicaid Information Section is a part of the MDS assessment Resident Assessment Instrument (RAI) in Texas and must be completed for Medicaid reimbursement. The Long-Term Care Medicaid Information Section must include the last name and license number of the registered nurse (RN) assessment coordinator. (d) The Basic Tracking Form must include: (1) the signature and title of each licensed nurse or health care professional completing any section of the MDS assessment for Medicaid reimbursement; and (2) the section(s) and completion date(s) corresponding to the signature of the nurse or health care professional. (e) Each individual signing the signature section on the Basic Tracking Form is certifying that the information entered on the MDS assessment is accurate. A facility that submits false or inaccurate information is subject to sanctions under Subchapter G of this chapter (relating to Administrative Actions and Sanctions). (f) If the nursing facility recipient is a hospice recipient, the nursing facility must comply with the requirements of 40 TAC §19.1926 (relating to Medicaid Hospice Services) and maintain in the recipient's clinical record copies of the completed Texas Medicaid Hospice Program Recipient Election/Cancellation/Discharge Notice (Form 3071), and the DADS Medicaid/Medicare Hospice Program Physician Certification of Terminal Illness (Form 3074). (1) The nursing facility must acknowledge a recipient's admission to hospice services on the Special Treatments, Procedures, and Programs section when completing an MDS full, comprehensive, or quarterly assessment.
(2) An MDS assessment indicating that a recipient has elected hospice services is not processed until the Texas Medicaid Hospice Program Recipient Election/Cancellation/Discharge Notice (Form 3071), and the DADS Medicaid/Medicare Hospice Program Physician Certification of Terminal Illness (Form 3074) are received by the Texas Medicaid Claims Administrator. (3) When a recipient is admitted to hospice and there has not been a significant change in condition, a significant change in status assessment does not have to be completed. The recipient's next scheduled assessment may be used. (g) Each nurse's license number submitted on the MDS assessment, Long-Term Care Medicaid Information Section, is validated with the Texas Board of Nursing or as applicable as a nurse compact license with the licensing state. An MDS assessment is rejected for Medicaid reimbursement if an invalid or delinquent license number is submitted on the MDS assessment, Long-Term Care Medicaid Information Section. (h) Nursing facility staff must complete the HHSC-approved MDS training in accordance with this subsection.
(1) The nursing facility RN Assessment Coordinator must complete the HHSC-approved online MDS training course prior to completing an MDS assessment for Medicaid payment. All other staff completing the MDS assessment for Medicaid payment are encouraged to take the MDS Training prior to completing the MDS assessment.
(2) The nursing facility RN Assessment Coordinator must repeat the MDS online training every two years. A certificate of completion is issued at the conclusion of the training. (3) If the nursing facility RN Assessment Coordinator does not complete the MDS training every two years as required by HHSC, the license number of the RN Assessment Coordinator is not accepted into the state database and the MDS assessment is rejected by the Medicaid claims administrator. (i) An admission assessment, a quarterly assessment, significant change in status assessment, annual assessment, significant correction to a prior quarterly assessment, or a significant correction to a prior annual assessment establishes a RUG-III group. (1) A significant change in status assessment, which requires a comprehensive MDS with Resident Assessment Protocols, must be completed by the end of the 14th calendar day following determination that a significant change has occurred. (2) A significant change in status assessment resets the schedule for the next annual assessment.
(j) Permanent medical necessity is determined by DADS in accordance with 40 TAC §19.2403 (relating to Medical Necessity Determination). (k) When correcting errors in an MDS assessment, the nursing facility staff must use the MDS Correction Policy in Chapter 5 of the Minimum Data Set, Resident Assessment Instrument User's Manual, published by CMS. (1) Documentation must be maintained in the clinical record to support the corrected MDS assessment form and be available for review by the OIG staff during MDS utilization reviews.
Form 3074 September 2014-e

(2) The Correction Request Form attestation of accuracy of signatures must contain the RN assessment coordinator's and Director of Nursing's signatures, and the date the correction was completed. (3) A correction to a RUG reclassification error identified during an on-site review is considered an assessment error as described in subsection (r)(2) of this section. This does not negate the facility's responsibility to make quality of care corrections pursuant to the CMS MDS Correction Policy referenced in this section. (l) The MDS assessment establishes the rate(s) at which the Texas Medicaid program pays a nursing facility or hospice provider for the facility's hospice residents to support the care the nursing facility's residents receive and any information on the MDS RAI is considered part of each corresponding claim for Medicaid reimbursement. (m) Prior to entering a nursing facility for review, the OIG identifies a population of paid claims from which a sample is drawn.

(1) The population is defined as claims associated with RUG classifications: (A) paid to the nursing facility, or hospice provider for the facility's hospice residents, for a specified time period; and (B) that meet certain criteria, such as dollar or claim volume, as determined by the OIG. (2) The OIG identifies the population of paid claims, along with their related RUG classifications and MDS assessment claim forms, from which a statistically valid random sample is drawn for review. The sample generated is a statistically valid random sample generated at a minimum confidence level of 90 percent and a maximum precision of ten percent. Related extrapolations are done at the lower limit of the applicable confidence interval. (n) Utilization reviews are conducted in accordance with this subsection.
(1) OIG nurse reviewers conduct unannounced on-site MDS utilization reviews of nursing facilities.
When is it time for Hospice Austin care?At any time during a serious illness, it is appropriate to discuss all of your care options, including hospice. Based on your needs and wishes, there are three ways we can serve you:Hospice Austin provides comprehensive, specialized care to patients and families living with an illness with a life expectancy of six months, if the disease runs its expected course.
Medicaid Hospice Physician Certification Form
Patients may receive hospice care longer if needed. If their condition improves, they can be discharged from hospice care and return to curative treatment.provides expert help with pain and symptom management for individuals who have a serious illness. Hospice care does nothing to hasten or postpone death. For some patients, there comes a point when treatment is no longer working. Continued attempts at treatment may even be harmful to patients already in a weakened state.Research published in the Journal of Pain and Symptom Management found that terminally ill patients who received hospice care lived on average 29 days longer than those who did not opt for hospice near the end of life.Many hospice care patients experience less anxiety by refocusing hope on what might be realistically achieved in the time remaining and spending quality time with loved ones.
Nj Medicaid Hospice Forms
Hospice care is covered by Medicare, Medicaid and most private insurance companies.We are contracted with most private insurance plans, including Aetna, United Healthcare, Humana, Tricare, Cigna, Sendero, Ambetter, Seton Health Plan and Blue Cross Blue Shield (except for the HMO Blue Advantage policies). Each of these policies will be subject to the benefits assigned by the carrier. We are also contracted with the VA in Temple for coverage.Medicare Part A covers 100% of hospice care for patients receiving care in their homes, nursing facilities, hospital general inpatient, or at Hospice Austin’s Christopher House.Like Medicare, traditional Medicaid covers hospice care at any location and at any level of care along with any supplies and technical and professional services related to the terminal diagnosis. Medicaid coverage includes the Children with Special Health Care Needs program through the Texas Health and Human Services Commission. Hospice Austin is contracted with Texas Medicaid for Travis, Hays, Caldwell, Bastrop and Williamson counties.
Texas Medicaid Emergency Only Care does not cover hospice care and Texas Medicaid is billed when the patient has a Medicaid HMO through a private insurance company.As a mission-driven nonprofit organization, we provide care to all who need us, regardless of a patient’s ability to pay.